Adapt health systems to support non-doctors, nurses and community health workers to manage chronic conditions in low and middle income countries
NEW DELHI, DEC 6. Chronic conditions such as cardiovascular disease and cancer are now the leading cause of death worldwide, including in many of the world’s poorest countries – where doctors are scarce. A team led by researchers from Mount Sinai and supported by New York University and the George Institute for Global Health looked at the existing body of research to glean how nurses, community health workers, and other non-doctors can best treat these multiple conditions worldwide – and how to adapt health systems to make it happen.
The study systematically reviewed all previous research on the subject of non-physician health worker (NPHW) care for chronic, non-communicable (not infectious) diseases in LMICs. They then reviewed the health system factors in each study that made such care better or worse. They sorted and analyzed the results in six categories: service delivery, workforce, governance, information systems, medicine access, and financing.
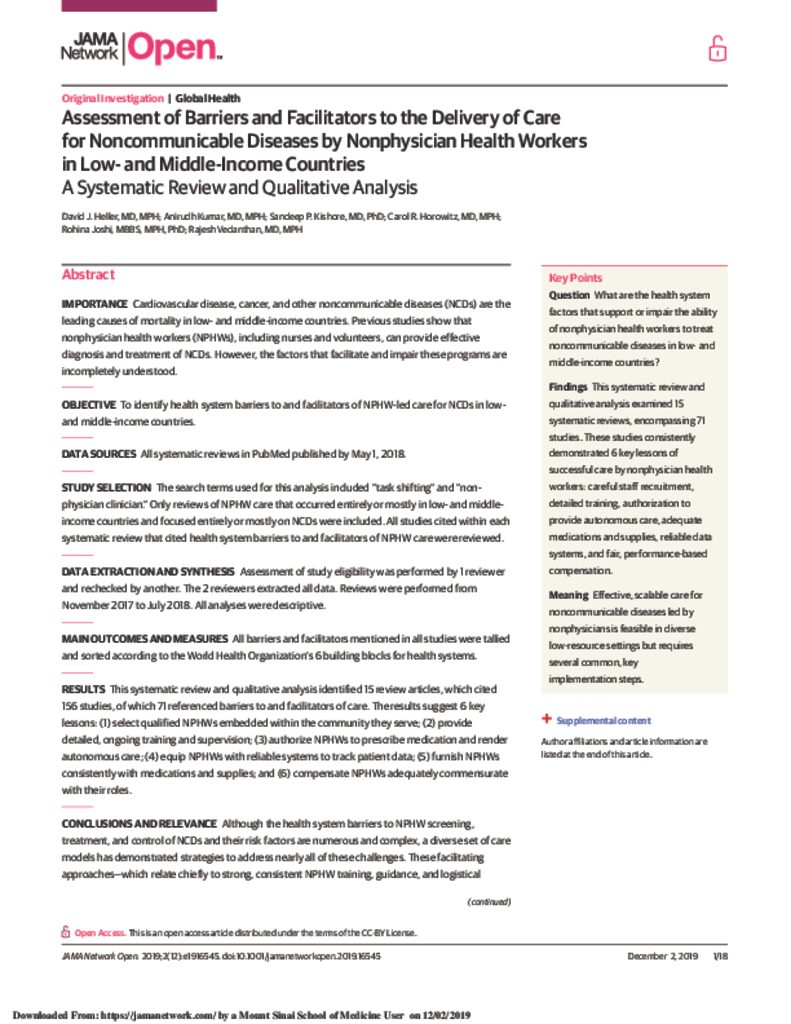
The findings have now been published by JAMA Network Open in a paper entitled “Assessment of Barriers and Facilitators to the Delivery of Care for Non communicable Diseases by Non physician Health Workers in Low- and Middle-Income Countries.” The paper includes a review of all studies relevant to the topic published by May 1, 2018 and included 15 reviews citing 71 studies, of which 11 were from India.
The authors identified six key factors to help non-doctors provide this chronic disease care. First, choose skilled workers from among the local community; second, give them appropriate training and supportive supervision; third, allow them to prescribe medications. Fourth, give them adequate data-tracking systems; fifth, given them adequate supplies and medications; and lastly, pay them appropriately for their work.
The research is interesting and timely as a rising wave of chronic, non-infectious diseases like high blood pressure and depression is now surpassing infectious conditions as the leading cause of human disease. In regions with doctor shortages – including the United States as well as low- and middle-income countries worldwide – these results can help build primary care programs to control this epidemic.
Talking about the research, Dr David J Heller of Mt. Sinai said
“Chronic diseases are the world’s leading cause of death, but many health systems are not prepared to deal with them. The world needs to build new, creative primary care programs to treat these multiple conditions – using nurses, health volunteers, and other workers in tandem with physicians. Our work suggests several ingredients to ensure that such programs succeed.”
Added Associate Prof Rohina Joshi of the George Institute for Global Health, who is a co-author to the study, “India has 0.7 doctors for every 1000 individuals, this is less than the minimum recommendation of 1doctor per 1000 individuals suggested by the World Health Organization. Added to this is the rural-urban mal-distribution of doctors in India where 70% of all the doctors reside in cities while 70% of the population live in villages. Sharing tasks between doctors and non-doctors will improve access to health care.” Associate Prof Rajesh Vedanthan, from New York University added “This study will help policy makers understand the system related barriers in delivering care for chronic disease in India and other LMICs. It would also help countries provide universal health coverage”.
Those involved in the study included Dr Heller and Prof Horowitz of the Arnhold Institute for Global Health, Icahn School of Medicine at Mount Sinai, New York; Dr Kumar Department of Medicine, New York University School of Medicine, New York; Dr Kishore Department of Medicine, Brigham and Women’s Hospital, Boston; Department of Population Health Science and Policy, Icahn School of Medicine at Mount Sinai, New York; Associate Prof Rohina Joshi of The George Institute for Global Health, New Delhi, India; University of New South Wales, Sydney, New South Wales, Australia; Associate Prof Rajesh Vedanthan Department of Population Health, New York University School of Medicine, New York.