Scaling-up The Competency of Primary Care Workers to Manage Epilepsy by Task-Sharing (STOP-Epilepsy)
Background
Most people in low and middle-income countries (LMICs) such as India cannot access quality healthcare. A paucity of healthcare workers, particularly specialist physicians, is one of the main reasons. Task-sharing approaches in LMICs were recently reviewed and found to be a viable option to improve disease outcomes while also leading to capacity building and cost savings.
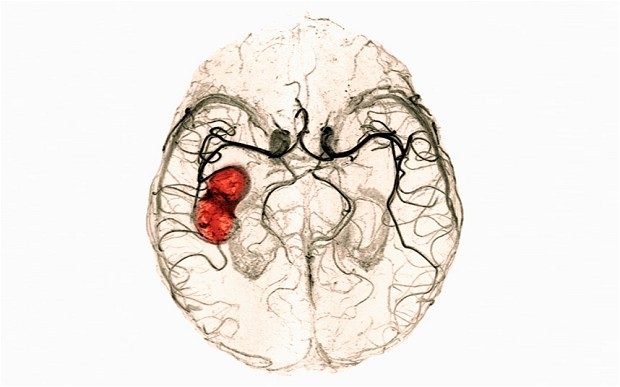
Epilepsy, one of the commonest neurological disorders, affects 50 million people worldwide, of whom, a fifth live in India. It accounts for 14 million disability-adjusted life years and 1,26,000 deaths worldwide each year. The treatment gap is high, almost 50-80% in India. A professional resource gap is one of the important reasons for the treatment gap. There is a lack of specialists to manage epilepsy across the country.
Our previous study points towards an unmet need for a comprehensive approach towards epilepsy care in the community, which should essentially include capacity building among care providers, raising community awareness and strengthening health systems. The current study, STOP-Epilepsy, is ideally suited to test a task-sharing initiative in managing epilepsy.
Aim
To determine whether an epilepsy-specific, community-based, primary care intervention comprising healthcare provider education, community awareness and home care by ASHAs, enabled by a technology-driven, mobile-application (EMADS) based decision support and communication system leads to increased chances of remaining seizure-free for at least one year in those receiving the intervention.
Research Methodology
A before-after study design for this hybrid, implementation and interventional initiative for provision of epilepsy-specific primary care services to the community at three sites across India. Evaluation will be done by mixed methods, including both quantitative and qualitative methods, during an initial observational phase with the subsequent interventional phase. We will follow complex intervention guidelines to develop, evaluate and report the project. Training young physician researchers to ensure sustainability will be an integral component of the study.
Impact
Task-sharing approach could be expanded to other non-communicable diseases. The economic analysis of the study will inform the resource needs and assist policymakers in future planning. If successful, the model could be proposed for adoption in several LMICs.
Current Status
The study is in the observational phase.









